FULL TRANSCRIPT OF PODCAST LISTED BELOW BIO
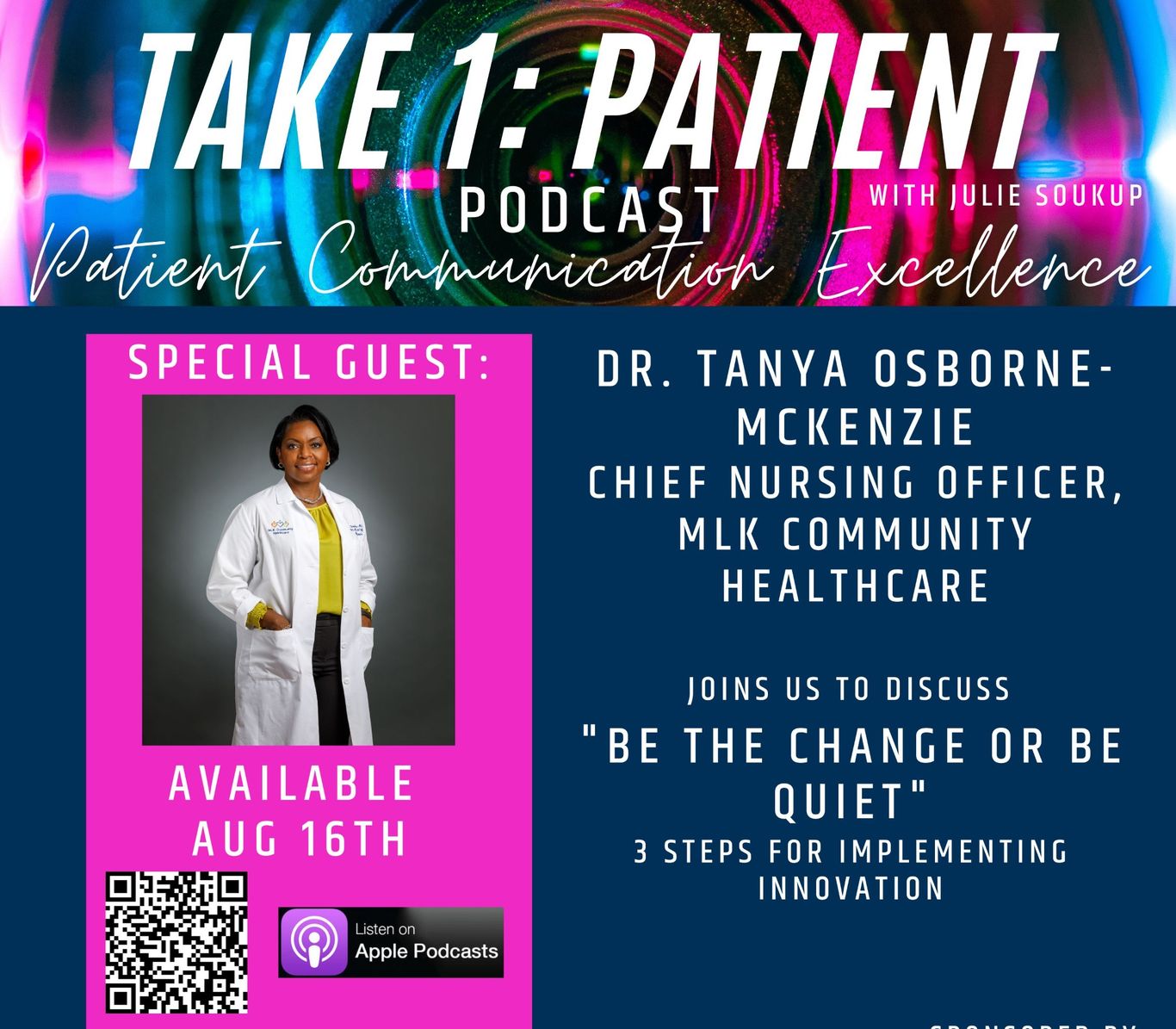
Dr. Tanya Osborne-McKenzie
"Be The Change or Be Quiet"
Dr. Tanya Osborne-McKenzie joins Julie Soukup, Chief Nursing Officer of MLK Community Healthcare to discuss her experience growing and learning the specialty of leadership. She discusses ways to create change in a hospital system with 3 key factors. 1.) Make a business case for the quality of care via research and data 2.) Speak to the why 3.) Patient at the Center of business.
Transcription of Podcast
Julie Soukup 0:01
All right, my name is Julie Soukup. And I'm here with another episode of take one patient. I am so excited to be talking today with Dr. Tanya Osborn mackynzie. She has a wealth of experience and knowledge, and is currently the CFO of MLK community health care. But a lot of education and a lot of different roles. And a lot of work has kind of gotten into where you are today. So I would love to first have you just talk a little bit about your experience. And really kind of what got you to where you are at your current role now.
Tanya Osborne-McKenzie 0:34
Okay, thank you, Julie. As you said, I'm Tanya, I am a nurse and I started nursing about 32 years ago, I did not want to be a nurse. And in fact, my plan was to be a nurse until I figured out what I wanted to do with my life. I actually had lots of opportunities to go to school and went kicking and screaming till until finally I just decided, you know, all of the I had all the prerequisites. So I went ahead and got into the nursing program. But that was the plan to start there figuring out what I wanted to do. When I started as a nurse at the bedside, I worked in the ICU, I took care of critically ill patients and actually started to really enjoy what I was doing. I also started doing some other things I do adjunct faculty, teaching folks in clinical space, I also started teaching classes at the hospital ACLs BLS different types of classes to my peers, and really just started really enjoying the work that I did. I continued at the bedside, I go to work, sometimes you don't go to work, and you look at people and you're thinking, Oh, I couldn't do that, oh, I shouldn't do that. So I actually talked to my mom who lived with me at the time. And I would go home and I would complain, well, you know, they did this, they did that. And what she told me was, you know, Tanya, you need to be like Gandhi, you need to be the change you want to be, or you need to be quiet. And so that's what really made me decide, you know, instead of complaining, what can I do, and I applied for a director position for my first real formal leadership role. And when I applied for that position, I and I didn't get it. Right, I applied for director position, I did not get it, I felt like I really should have, I felt like I really should got it. And so after you go through feeling sorry for yourself, I went back to a friend and colleague of mine who was on the interview panel, and I asked her what what happened. And she said, we really thought you would do a great job. But you know, what you behave like what you are is a really strong clinician, but you didn't you looked as if you had not seen the job description at all. So it's like, okay, so I went back to my life, I started going back to school to get my baccalaureate degree. And about 18 months later, another director position opened up. And at that point, one of the floors that I was teaching on their leadership, the assistant nurses there, this is that nurses, their their educator, their case manager, they called me up to meet with them. So I went up to meet with them. And they asked me if I would apply for the director job on that floor. And I part of it, you know, still feeling a little disappointed that I didn't get the first opportunity I applied for but also, what I told them was and this was factual. It was a joint replacement spine and post op floor and I said, I don't know, orthopedics, I worked critical care. And Lourdes who was the educator, she told me, she said, we have orthopedic nurses, we need a leader in between what I was told by my friend and colleague before and what Lord has just told me there. And finally I had this epiphany that leadership is, and that's a specialty in and of itself. And I was looking at it all wrong. I mean, and so that's when I really started to understand leadership as a specialty. And there's a certain set of skills that you have to have to be a good leader. And so with that, I did apply for that position. I was awarded that position. And so we had, I was the director. So I went from literally that Friday, I had an open heart surgical patient that was taken care of. And that Monday, I was now the Director of what was really a joint spine and post op floor. I miss some steps in there. So I you know, I was never I did relief charge but I was never a formal charge nurse. I was not an assistant manager or manager, I went from a staff nurse to a director. So there were some gaps in my education, right, some gaps there in my knowledge, and so I continued my education, so I finished my baccalaureate degree. And then I went to get my masters and I decided I wanted to honor nursing and wanted to make sure I obtained the Masters in Nursing. But I also recognized at the time that nurses one of the things that we could be a little stronger in is being able to make a business case for quality. And so I wanted to be able to understand the business part of a sale So ministration, so I earned an MBA as well. And then one is I'm kind of a nerd, I just enjoy school, but also wanted to ensure that I really understood my job and the role and decided I would go back to school to get a doctorate. And at the time, I was interested in getting a PhD. But the PhD is really about research. And the work that I do is in the practice, arena, and so spoke to some friends and colleagues, and they talked to me about doctrine and nursing practice DNP. And that focus is really around putting the research into practice into his environment. So that was really interesting to me. And the University of San Francisco has an executive leadership doctorate in nursing practice degree. And so that's actually what I where I went. And that's where I earned my executive leadership DNP. Some of the benefits of that, because I get a lot of times people say, Well, what, what is the DNP? And what'd he do? What did you learn, but some of the things besides, there's foundational knowledge, right? In executive leadership, there's also finance at a higher level, and lots of work around change management, because if you're going to bring that research into practice, you actually have to understand the steps of change management, you and especially, right, we want to use the evidence, the science that that we want to not just conjecture, and this is what I think. But actually, here is really the evidence that shows if you do this, you will get the outcomes that you want. So I after I graduated with my DNP, I switched jobs, because I just really wanted to see if I could replicate what I had done at the first hospital to the next hospital. And I felt like I was successful there. And then there was an opportunity at Barrow Neurological Institute, which you know, is world famous. And and so I transferred to I went to work there at St. Joseph's to be the senior director at Barrow, Neurological Institute, Senior Director of neuroscience nursing. And that was a really a great place to be I love Barrow cannot ever say enough good things about the level of
caring for the patient, as well as the level of science that they want to bring to that area, the innovation that we have there. It's just it was a fascinating place. We went through as soon as we as soon as I got there, I think five months later, we went through COVID. And so while I was there, I shifted and I was very honored to be given the Assistant Chief Nursing Officer of position for St. Joseph's Hospital, which Pharaoh is a part of. And then while I was there, I really thought a lot about the fact that I've been doing I've been in leadership for a long time. And I always thought I would I was happy as a director, but then I realized that, you know, there was a little bit of, you know, imposter syndrome of sort of like, How did someone who can't who started this journey as an adn grad? And how do I how can I imagine myself being a chief nursing officer someplace? And but then I at that point, I started to realize I could do it. And not only could I do it, but I shouldn't do it. And so I really wasn't actively looking for a role, however, and that's the way life is right. What happened was this, this roll here. I knew someone who had been at this hospital before, and had told me to talk to him about the hospital what they were doing in Martin Luther King Community Hospital here in LA. And where I met this community, there's a desert of physicians, they we could actually use at least 1200 more physicians in this area in this. We don't have, and this is a it will. kch is a private public partnership. And the goal is to care for the patients in this underserved community. Dr. Batchelor, who is our CEO here, very much committed to providing the same level of care here in the safety net hospital in this community that people would find in any other hospital in a more affluent neighborhood. And to that end, we are working on achieving magnet which is Nursing Excellence that some people may not expect to see in a hospital like this. We've recently just received the Joint Commission's certification for advanced diabetes care which less than 70 hospitals, not safety net hospitals, but less than 70 hospitals in the country have that designation. So we are very much on a journey to provide excellent care to the folks in this community, the people you would think would need it the most. We've just started a street medicine program. So we go out on the streets to take care of patients who are unhoused. So this is one of the things, some folks, you know, that it's a relatively small hospital center, 31 bed hospital, so people, you know, I've had some people say, Oh, my gosh, you're moving from this big hospital to the smaller hospital. And I like to tell people, it's a smaller hospital, but it's a really big job, it is a really big job.
Julie Soukup 10:33
Yeah, well, and, and, and, I mean, especially now that you're starting to be able to have a different perspective, from, you know, even Barrow to a situation such as that, you know, and bringing that kind of wealth of knowledge of different ways to start implementing and making changes and places a hospital that maybe didn't really have that kind of focus before. So you've really talked when we had spoken before, and I thought it was really, you know, spot on as far as like to for for other people that are really looking at, okay, I might not have a chief nursing officer role, I was a director, or things along those lines. But I do want to start having an impact, I do want to implement something I want to try something out, especially for, you know, we had met you with with working with medical memory with with St. Joe's and which is that HIPAA compliant app for video recording patients? So even we have a lot of directors that are like, okay, like, I want to I want to do this or I want to do something different. What are you kind of talks about some of the steps that you go through, when looking at trying to implement something, talk a little bit more about that, and what you've learned, even for someone that's a director that wanted to kind of start doing some of those things, or nursing wanting to start trying out something new.
Tanya Osborne-McKenzie 11:50
Right, right. So one of the things when in terms of my job, and this is what when I was director as well as now, because I did get my doctorate while I was a director. I've had it for about 10 years now. But one of the things that we focused on that we really focus on what that DNP is pulling that science into pulling that research into the the workplace. And some basic a process of basic process for improving or making changes is really first understanding the reason for the change. Really, why is it that why is it that I'm going to do this, but the so what, I'll give you an example, since you did bring up medical memory, when I was at barrel, we decided that, you know, we know that there's a lot of research that talks about the patient experience and how it is related directly related to patient outcomes, right. So if I improve the patient's experience, then I can improve the patient outcomes. And if you're a nurse, as a nurse, we know that our job is literally and I think it's on the a and a policy statement actually says that nursing is the diagnosis and treatment of the human response to actual or potential healthcare problems and or needs. So if our job as nurses is to diagnose and treat the human response to any healthcare problems or needs, and we want to make sure that we do that, then we need to use the science. And if the science then says that patient experience is directly related to outcomes, if we improve the patient experience, we improve their outcomes, then we actually have to figure out how are we going to do that. So starting with, what's our reason for action, our reason for action is to improve the patient experience so that we can have better outcomes, we can improve our patient outcomes, which is something everyplace wants to do, of course, we wanted to do that arrow, and then you look at what your current state is, and what your target state is. In this case, it's easy, because we have H cap scores, which most hospitals will look at. So we targeted one part of our H cap scores, which was RN communication. So we wanted to improve the nurses communication with the patients. Because if we can improve the nursing communication with patients, so if you think of just building relationships with the patients, the patients feel more comfortable telling the nurses or their physicians, what is happening with them what their needs are, they're also more open to listening to us and helping and collaborating with us to help improve their care, right. So we look at what's the reason for action, we look at our current state, and then what our target state was. So in this case, we looked at what our current state was for. Overall, our composite percentile how people want it, you know, would they want to come back? Would they recommend being at barrel recommend being on those units? And then we looked at our current state of communication with nurses in general for me specifically for our H cap scores for each of the units. So then you look at the gaps. What are the gaps? Well, one of the gaps was that it was hard to time when the fan only for those patients with be there. And when the nurse would be in the room or when the families who are there and the the doctors would be there. Another one of the gaps is that we knew that people forget about board, you know, they remember about 40% of what you tell them in the hospital, right, you're not at home, you're sleep deprived, you're actually in the hospital because you're sick and you're stressed, you don't remember a lot of what's going on. So some of the science, we looked at what was happening with the physicians who were currently using medical memory. And we looked at the data and the physicians that were using medical memory, their individual patient experience scores were vastly higher than what we saw with the physicians who weren't using medical memory. So we believe that if we use medical memory for nursing, that we would get that same result. So our we did a PDSA, which basically was, we started to sign we started to register the patients who were on those
on our units in barrel, we would register them with medical memory. And then the expectation was that the nurses would every day would just give one small like one minute medical memory update. So they would do one video, often they'd be in the room with the patient, they'd have the medical memory camera on the patient, and they would say, you know, I'm making this up. But something like this is your mother today she slept well, last night. Today, she's going to have a CT scan, the doctor will be in later to give her the results. Just really brief. Sometimes the the message was something like I remember this one where there's one patient that they changed the time of the patient's surgery, and the nurse just put up a video showing that patient and saying that, you know, the your mother's time for surgery was changed. It's going to be an hour and a half earlier. Right. That was it. But that was one of the videos that we received the most input about because the family was so grateful just to get that to get that information. Yeah, the interesting thing about doing this was I told you, I started working at barrel at St. Joseph's in 2020. I started working five months before the pandemic started. So here's the interesting thing about this. And this is why it is so important to that, that science and use a strong change management process to guide what you do. Because, right as we started this COVID happened. And if you remember when that first started, we didn't let anybody in the hospital. No one. So if you look nationally, most everybody's scores for communication dropped. In this case, and then remarkable thing about this was our scores actually went up. Yeah. So I know specifically for those med surg, tele floors, where we started with a baseline in neuro telemetry we are average was both communication with nurses, our average was 16%. And it actually went up to 45%. By by the end of the year. So using the science, understanding where the gaps are, having a strong implementation process, those are the kinds of things with change management, that really helps a great deal and something that we definitely learned during that time. But a lot of that is where what I learned from experience and also just, you know, and from school, to be honest, yeah.
Julie Soukup 18:30
It breaks it down. Yeah. I mean, into, just as you said, is was, you know, starting with a patient, having your why is great, like, great. This is why I want to do it. But taking that okay, well, what is the business case? And hospitals are still a business, you know, people don't know, man, but it still is, well, what is the value it's going to provide? And what is the financial benefits going to provide? If you're saying, you know, patient centered a patient focus with that, you know, it's easy to kind of build the business back versus just, oh, it's simple. So this would be great. And so leveraging H caps or leveraging, you know, you know, patients readmissions or outcomes or anything like that, what's, what's the business there? And I think those kinds of even backwards steps I'm almost visualizing really helps IT support more of that leadership is a practice of what's the why even try it not just for the patient, but why to try it for a hospital.
Tanya Osborne-McKenzie 19:23
Exactly, exactly. There's a book that I read, it's called, so good, you can't take notes so good. They can't ignore you. And the reason that I think of that, but I think about back when I first started nursing, and I absolutely did not want to be a nurse. And so what he did, I can't remember the author's name, but what he posits is that one of the things that we have right now everybody wants to have a job that they are passionate about, and people feel like they have to have a job that they're passionate about. And, you know, for example, my husband, if he had a job that he was passionate about, he would be a professional golfer. He's passionate about golfer he's not Great golfing, we would be hungry. This author posits is that if you are, if you start, what work you're in right now, whatever work you're in, the more you learn about it, the more you get interested in it, the more you learn about it, the more you become an expert in that area, the more people start to ask you about it and asks you to offer them your expertise, the more you actually start to really enjoy the work, which, frankly, is what I believe happened with me with nursing. Now I just, I read that book, like 20 years after I became a nurse. But I really do think that there's a lot to that philosophy. And so I say that because with nursing leadership and understanding that that truly is a specialty, the more you learn, and the more competent and proficient you become at those leadership skills, the more you enjoy that work, right,
Julie Soukup 20:54
right. Well, and as you kind of even said, is, you know, first, like, there's tons of books and so much data that's available, to kind of even start becoming an expert at just learning more, even in your specialty to help make those kind of, you know, process improvements or implementation improvements to you know, like that that are available, you know, how do you how do you when you are like you like, we can keep using medical memory as an example of different things. How do you go about what, okay, so now you have the business case, now you have the data, you're wanting to try something new, especially like video recording? And that's how do you go about when people then are resistant, or nurses are resistant? Or even, even the other way, leadership was more resistant? How do you break down those barriers? Knowing the research, knowing the data, knowing what you're trying to do? Great, we got it all buttoned up. But how do you how do you how do you how do you handle those type of situations,
Tanya Osborne-McKenzie 21:51
and you will get resistance, you know that even with any type of change management, your any change, you're gonna get resistance, I mean, it can be the best. I mean, it can be personal level, right? I want I need to lose weight, I need to have a healthier lifestyle. I know, that's what I want, it's still hard. So there's always going to be resistance, right? So with with, but just like with dieting, where I understand why I want to do it, and I own it, that's the same thing with any kind of changes that you can't have that change can't be in a vacuum, it can't just be me and my office, this is what we're gonna do, and then go out and do the change. Just like I owned the diet plan, my healthy lifestyle plan, you have to get the team to own the change process, because then when it gets hard, the team owns it, we can still work our way through it. And so what I mean by that is, for example, with, right making the business case for quality. So if I'm looking for funding, I need to be able to make the business case with the finance folks of they own the change. I'm actually doing a change here right now that I want. And that was the first thing that I did was I went to the finance folks and explained what I wanted, right? My reason for action, like why am I doing it, where we're at right now where we'd like to be right, and then where my gaps are. And so you know, this is one of the things that I think we can close the gap on. And so once I'm able to partner with the CFO and his team, then I also I'm talking to my nurse leaders, we bring in some staff nurses as well, because we need everybody to own this process. So we kind of talk about the why we want to do this and hear what they have to say. And then I can bring up well, again, here is what here then they can help with, here's the why the reason fraction, I can give them the data for the current state, here's where we'd like to be. They all help with gaps. Here's the process most I've never had a position where when we looked at when I bring in the team to bring the gaps, if we've already started looking at the data, or even when the folks you know, when the team starts to look at the evidence, look at data. That, right if we're looking for evidence based practice, then we're all going to, we'll get we'll get to what we all want, right? And we all own it. But you have to bring those folks in early. You can't go to somebody, you know, think about that. Right? My husband comes to me and says Tony, you need to lose weight. Yeah, well, different stories. Oh, I need to lose weight. Right.
Julie Soukup 24:22
Yeah. That kind of thing. Yeah. So for when even like, Okay, you're going to nursing leaders or, or and someone's like, well, I don't I don't, I don't think this is going to work or I don't think I mean, I guess that's what you're saying is that's why you have the data to support it. And that this is what we're testing. This is where it's shown before, like, but even when you study people like well, there's another way we couldn't do it. I mean, how do you kind of get them even to be on board to own it or say, well, let's at least try it or how do you kind of go about that with with even those stragglers or once?
Tanya Osborne-McKenzie 24:56
No, because you will always have those and so when you look at the gaps, there's usually lots of gaps, right? But we have to prioritize what we're going to do first. And so it doesn't mean that what they're recommending is any more correct than what you're recommending. So what we usually do is we list the, the gaps, and we do a PDSA, right? process we look at, we do a cycle of change, and I think of it really, I actually I use this as an example all the time I think about the, you know, the iPhone, right? Because what the iPhone did for us, and the reason we're on like, you know, what is an iPhone 13. Now, they gave us an iPhone, that was good enough. And then we all said, let's, you know, we want this, we want that, then they go back, they give us something that's better. Here's our iPhone two. So that's why it's always a cycle. It's not, you know, it's not, here's the change, boom, we're done. It's always a cycle. And so sometimes in in healthcare, especially, we want the solution right away. And what I remind people is, it's a cycle. So we start with this, we get incrementally better, right? Now, let's add this next part, and get incrementally better, because we're always trying to, and that's why that, you know, perfection versus excellence. If you shoot for excellence, you can continue to get improvement you to for only perfection, people tend to get really frustrated, because how often can you get to perfection every day?
Julie Soukup 26:31
And I think it goes back to what you were saying earlier, is it It truly is a practice and and as you're even describing that is, okay, great. This was phase one. Now let's go back, let's phase two, let's go back, like let's continue to, to strengthen and improve, but you know, it's a practice, we're not going to always just have it like immediately like this is the magic bullet, because exact magic bullet that would be easier
Tanya Osborne-McKenzie 26:54
to write everything in healthcare changes, right? We hope it's always improving. It's always evolving, evolving, people are not stagnant. So they are going to continue to change. So we have to continue to evolve and change as well.
Julie Soukup 27:08
Right now? Absolutely. Well, thank you, for all of all of your intellect and all of your experience, especially as you helps you know, with medical memory, kind of getting those things through. But I think you bring up kind of, again, back to those three things of, you know, making a business case speaking to the why and then really keeping that patient at the center as you're kind of planning things out. And I think that that is great advice for anyone looking at implementing well, not even necessarily in a hospital just in anything. samples. And I you know, I know, like a lot of people kind of thinking about that in those those simple steps is, okay, great. Now I have kind of a plan of action, if you will, to kind of help support change in those things. So, um, yeah, I really appreciate you taking the time to be on our call today. Is there anything kind of you want to add as far as last nugget?
Tanya Osborne-McKenzie 28:02
I don't think so. I think you kind of wrapped it up for me, but I appreciate having the opportunity to be able to present some of my thoughts. So thank you for that. Yeah, absolutely.
Julie Soukup 28:10
So great. Well, thanks again and have a good rest of the rest of your day. Thanks, you too.
Transcribed by https://otter.ai
© Copyright. All rights reserved.
We need your consent to load the translations
We use a third-party service to translate the website content that may collect data about your activity. Please review the details in the privacy policy and accept the service to view the translations.